Understanding OCD: A Comprehensive Guide for Patients and Families - II
By Aarogya Minds
What Treatments Are Used for OCD?
Currently there is no cure for OCD. However, with effective treatment, people can learn to manage their symptoms and restore normal functioning. Best practice guidelines for OCD recommend cognitive-behavioural therapy (CBT) and antidepressant medications for OCD treatment. While many people will benefit from using one or the other, those with moderate-to-severe forms of OCD often do best when both treatments are combined.
It is important that people get treatment specific to OCD from a Psychiatrist or qualified CBT therapist. This type of treatment may be available in either individual or group formats, and each format has advantages and disadvantages. While some forms of traditional psychotherapy may help other aspects of a person’s life (e.g. relationships) they are not effective for OCD. In addition to CBT, people with OCD may benefit from supportive counselling and marital or family counselling.
1.Psychological Treatment: CBT
Cognitive behaviour therapy (CBT) is widely considered the best psychological treatment available for OCD. Specifically, a form of CBT called Exposure and Response Prevention (ERP), is the most commonly used therapy in major health-care settings.
This treatment is based on some known facts about anxiety:
• Anxiety is a response to threat or danger.
·· People with OCD interpret certain situations as dangerous and therefore anxiety gets triggered. When something is perceived as dangerous, the fight, flight, or freeze response kicks into gear.
• Anxiety is adaptive and helpful. We need it to survive.
·· The fight/flight/freeze response is our body’s way of staying safe. For example, if a car is racing towards us, anxiety helps us to get out of the way quickly. Or, if necessary, anxiety prepares us to fight off an attacker coming towards us.
• Anxiety is not dangerous.
·· The anxiety itself is not a problem even though it may feel awful.
• Anxiety shows itself in three ways: Mental, Behavioural, Physical
·· Mental: thoughts like “something bad is going to happen”
·· Behavioural: actions like avoidance or compulsions
·· Physical: sweating, dizziness, breathlessness
• Anxiety cannot continue forever or spiral out of control; it will go down…eventually.
·· Sometime after anxiety has been triggered, there is an automatic response in our bodies that helps to restore a calm feeling.
1.A How does Exposure and Response Prevention (ERP) work?
In ERP practice, a person will expose themself to a situation that triggers anxiety, and then prevent the usual OCD response (compulsion or avoidance). ERP is based on the idea that problematic anxiety is often a learned process, and can therefore be unlearned.
In ERP, people confront feared situations in a controlled and gradual fashion with the help of a therapist. The first step is to make a list of feared situations. The items on the list are organized in a hierarchy, from least anxiety provoking to most anxiety-provoking. For example, someone with doubting obsessions might have a list that looks like this:
1. leaving the house without checking the door (40% anxiety)
2. leaving work without checking office door (70% anxiety)
3. leaving house without touching knobs on stove (90% anxiety)
The next step in ERP is to confront to the triggering situations listed in the hierarchy, one at a time, from easiest to hardest. The first exposure session, involving the easiest situation, is usually done with therapist assistance. These sessions can last between 45 minutes to 3 hours.
The person will then be asked to repeat the ERP frequently in order to reinforce the new learning: that nothing bad will happen. When the behaviour gets repeated enough times, a process called habituation occurs. Habituation means it gets easier over time!
As the person becomes less anxious in response to the easier situations, their confidence slowly begins to grow. More difficult situations from the list are introduced, following the same process, until the person achieves significant relief from their symptoms.
When a person only seems to have obsessions, without obvious compulsions, ERPs are tailored to obsessive thoughts. For example, a person with religious obsessions may “expose” themselves to their feared thought by writing it down on paper over and over again.
Sometimes, direct, or “in vivo“ exposure is not possible in the therapist‘s office. For example, for a person with fears of yelling out obscenities in church, the therapist might ask them to use “imaginal“ exposure. This is when a person imagines the different situations that provoke anxiety.
Self-directed ERP
For people with mild OCD, ERP can be done successfully without the help of a therapist. There are some very useful self-help books to guide this process. Please see a list of recommended self-help books for OCD and Related Disorders in the Resources section.
Is ERP effective?
Research shows that ERP can help a person reduce their OCD symptoms by up to 80%, and maintain this improvement over time. A person‘s success with ERP therapy depends on several factors, including motivation. Other factors include symptom type and whether other disorders are also present, like depression. Studies indicate that over 75% of patients experience some kind of improvement with ERP treatment.
1.B Cognitive Strategies
In addition to ERP practice, CBT also involves challenging the unhelpful interpretations in OCD (see Cognitive Theory) and promoting more realistic thinking styles. Using cognitive techniques, people can learn to identify problematic thinking patterns that contribute to OCD.
When cognitive strategies are used along with ERP, patients will usually start by paying attention to thoughts and feelings related to exposure situations. These thoughts are then explored to find out what makes the situation so upsetting. For example, some people with OCD have a tendency to overestimate danger (e.g. a belief that the likelihood of getting infection is very high by touching public doorknobs). Using cognitive therapy techniques helps generate more realistic and helpful interpretations.
There are several cognitive techniques used for OCD. The Thought Record is a key tool used in OCD.
Thought Record:
The Thought Record is a strategy used to challenge unhelpful, distorted thinking patterns. The goal of the thought record is to increase awareness of what we are thinking and then to examine the validity of our thoughts. Steps include rating moods, identifying thoughts that may relate to to the negative or anxious feelings, and looking at evidence that does or does not support the thoughts. Using thought records can help reduce anxiety by challenging the beliefs involved in OCD.
There are many other cognitive techniques that can be used in treating OCD. These include:
• Responsibility Pie
• Continuum Technique
• Probability Estimation
• Double-standard technique
and can be read about in some of the self-help books listed at the end of this guide.
How effective are cognitive strategies?
Studies show that using cognitive techniques alone, without ERP, can help reduce OCD symptoms. However, experts generally agree that using both cognitive and ERP strategies is most effective. When used together, cognitive and behaviour therapy tools work by learning new ways of thinking and behaving.
Treatment model for OCD
In CBT, we break this vicious cycle by challenging those negative interpretations and eliminating the compulsions/avoidance. The diagram below illustrates the cycle of OCD from a CBT perspective.
Cycle of OCD from CBT perspective
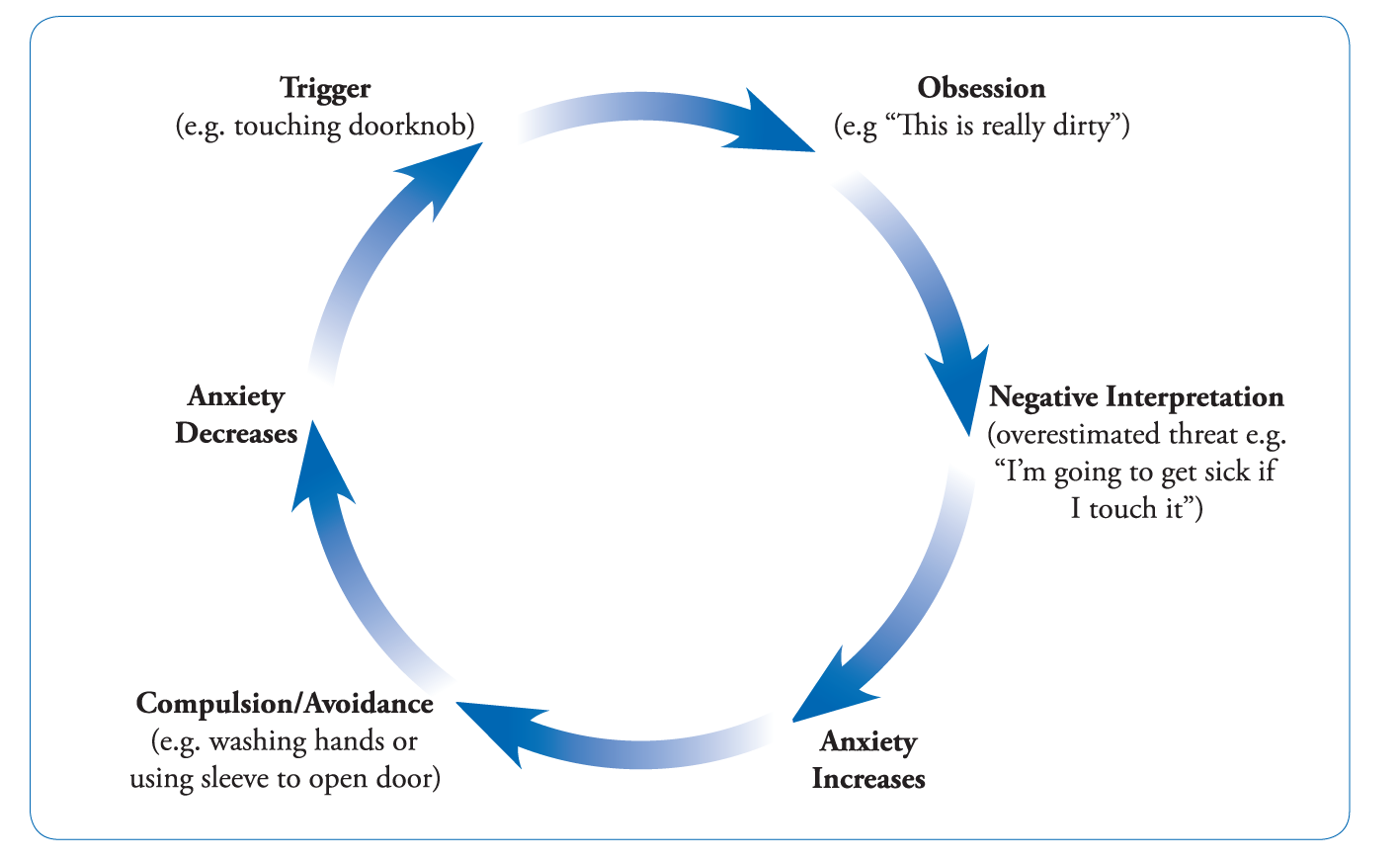
Cycle of OCD from CBT perspective
2. Medication
Medications, like cognitive behavioural therapy, can reduce the severity of OCD symptoms and may be an important part of any treatment plan. When illness symptoms are more severe, both types of treatment may be combined or provided sequentially.
The main class of medications is a large group of antidepressants called serotonin reuptake inhibitors (SRIs). These medications chemically block the absorption of serotonin by neurons, making more serotonin available to transmit messages in the brain. It is believed this change is associated with the improvement in OCD symptoms. Below we describe the three main subtypes of SRI medication:
SSRIs,
Clompramine,
and SNRIs.
Selective Serotonin Reuptake Inhibitors (SSRIs) :
This is a large class of antidepressants that work very specifically on the serotonin neurotransmitter system. These include the following:
These medications are considered 1st-line treatment for OCD for a few reasons. 1) There is a lot of evidence supporting their effectiveness in symptom reduction in OCD. 2) They are well tolerated in terms of side effects, compared to other medications for OCD. 3) They are relatively safe, compared to other medications for OCD.
Though these medications each work slightly differently and have different side-effects, they have all been found to be equally effective for OCD. It is very important to remember that one medication may work for one person and not another. It is common for people with OCD to try more than one medication in this category before one is found that improves symptoms with minimal side effects.
Clomipramine:
SRI Clompramine is the oldest and best studied SRI for OCD and depression and belongs to a separate class of antidepressants known as tricyclic antidepressants (TCA’s). It is found to be equally effective, and in some studies slightly more effective, than SSRI’s. About 80% of people taking it note improvement in OCD symptoms. However, it has a wider range of side effects that can make it more difficult to tolerate. As well, there are safety concerns for certain people. Because of this, clomipramine is often seen by treating physicians as a second choice after SSRIs.
Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs):
These are a newer group of SRIs that work on two neurotransmitter systems, serotonin and norepinephrine. These include venlafaxine, duloxetine and desvenlafaxine. They are also believed to be effective for OCD, although they have not yet been as well studied as yet as the SSRIs. Because there is less evidence supporting their effectiveness in OCD, they are usually seen as a second-line option after SSRIs.
When treating OCD with medication:
It can take 6-10 weeks to see any change in OCD symptoms.
Side effects often occur before improvement .
Improvement occurs gradually.
Doctors recommend staying on medication for 3 months to see if it’s helpful.
OCD usually requires higher doses of medication than other disorders.
Medication sometimes might not eliminate symptoms completely.
Medications for Augmentation
Addition of a secondary medication can be a very effective way to maximize response to an initial medication for OCD. These options are often non-antidepressants and come from a variety of classes:
Antipsychotic Medications
Antipsychotics have the strongest evidence for benefit as add-on medications to SRIs for OCD symptoms. Older options, including Haloperidol and Pimozide, may provide specific benefit for people with OCD and concurrent tic disorders, such as Tourette’s disorder. Newer antipsychotics (‘atypical antipsychotics’) including Risperidone, Olanzapine and Quetiapine have been found to be effective for a broader range of people with OCD. A newer generation of antipsychotics, including an option called Aripiprazole, shows some benefit, though further studies are needed.
Benzodiazepines
These medications tend to alleviate anxiety and help with sleep, though it is unclear if they reduce the core symptoms of OCD. One of the best options in this class is clonazepam, a relatively longer acting benzodiazepine which may alter the balance and availability of serotonin in the brain. Other medications in this category include lorazepam, diazepam, oxazepam.
Once Response is Achieved
A common question relating to medications for OCD and other psychiatric conditions is how long medication(s) need to be continued once there is an improvement in symptoms. It is generally recommended that individuals taking medication for OCD continue for at least twelve months and in some cases, two years or longer term.
There is often concern expressed that these medications are ‘addictive’ or that one can become ‘dependent’ on them over time. Neither of these ideas are true. Even if taken long-term, these medications are safe and it is fairly common for individuals to stay on them long-term without such risk.
A major complication of discontinuing medication is the significant risk of relapse, or return, of OCD symptoms. To minimize this risk, doctors recommend a number of strategies. These include gradual reduction of the dose over several weeks to months with close supervision, and regular follow-up with a health care professional, such as a therapist, to monitor symptoms. Doing cognitive behavior therapy along with medication also helps reduce the risk of relapse after stopping a medication.
How Does OCD Effect Family & Friends?
We are surrounded by others who we have an effect on and who affect us. And the more we care about one another the greater the effect. This might be especially true for people dealing with symptoms of OCD because they are woven through so much of life. All of the worries and repetitive behaviours that are a part of this disorder get played out within relationships and family life. People with OCD carry around severe and persistent worries in the form of disturbing thoughts, and once they have the thoughts they will try to do whatever they can to get rid of them. The anxiety feels intolerable. This leads to repetitive behaviours in the form of rituals that they hope will undo whatever has made them so fearful. The misplaced logic is clear to partner, family and friends, but they also clearly see their loved one’s distress, and so they accommodate.
Accommodation: Doing things for a person with OCD to help ease their distress. Accommodation may help in the short-term but makes OCD worse in the long-term.
And this is the problem. The loved one does not intend for the accommodation to become a pattern, but because the distress arises again and again, they find themselves accommodating over and over, until they find that the OCD takes over relationship and family life.
Thoughts for Loved Ones
When your loved one is first diagnosed you may find that a door has opened and hope arrives along with the possibility of treatment.It is important to let your loved one know that you have his or her back as they face their fears, while also being realistic that your own feelings will also show up. You may find that you feel resentment at the burden that OCD has imposed on your life, even sometimes feeling that it has stolen time that should have gone toward taking care of yourself or others.
The Challenge of Dealing with Accommodating, Rituals and Reassurance Seeking
One of the biggest challenges of OCD is the many ways it affects relationships within the family. People struggling with the symptoms of OCD often doubt many of the aspects of daily life that others sail through. For this reason they frequently look to the people closest to them for help in reducing their anxiety. At first it just makes sense to provide reassurance, “Yes, you turned off the kitchen stove.” But as it grows to include other things or in intensity, family members may become irritable. Yet, as a family member you may find that family life will slow to a crawl if you do not do things the way the person with OCD demands, by providing reassurance or participating in rituals. You may find yourself resisting these things some times and getting drawn in at others. You may experience guilt about how you are reacting at any given time and wish that there was a rulebook to guide your actions.
Another complicating factor is that each family member might have a different way of responding, with one person thinking that “tough love” and just saying “no” is the proper response, while another may feel that their loved one is just too distressed to ignore. This is not surprising. There is no one correct way to respond to OCD, especially when the person with OCD is not receiving therapy. Knowing this can be reassuring, but also confusing for family members.
Importance of Taking Care of Yourself
Here are some well-researched stress-reduction strategies:
1. Recognize when you are feeling stressed.
Some signs are increased heart rate and blood pressure, change in sleep patterns, difficulty concentrating, worry, irritability. You may even find that your mood is affected and you feel anxious yourself.
2. Mindfulness meditation.
Join a Mindfulness class to help manage stress with a daily meditation practice, which has been shown to help people manage stress.
3. Exercise.
All forms of exercise have been shown to reduce symptoms of stress, including walking, running, aerobic exercise, yoga, pilates. Recent research also suggests that exercise may be directly beneficial at reducing OCD symptoms.
4. Emotional Support.
Having the opportunity to talk with a non judgmental friend or family member is important when stressed. Joining a family support and education group can also be helpful to gain perspective.
5. Nature.
Research has shown that taking time to be in nature reduces stress. Even a short walk can be helpful.
6. No one is perfect.
This may seem obvious, but when there is suffering in a family you can lose perspective and feel that you should not take a break until everyone else is okay.
7. Professional counsellors.
Professional support, whether in the form of individual, couple or family counseling, can at times be the best help for dealing with stress. If you or someone else in your family is depressed, anxious or having thoughts of harming his or her self or others, this is the time to reach out to a professional.
8. Scheduling in time for activities that you enjoy.
Often when individuals are trying to support a loved one with a problem like OCD, they may forget to keep up their own interests and pleasurable activities.
Talking With Children
Here are some suggestions for helping children make sense of OCD in the family:
1. Provide information about OCD, its causes and treatments, using age-appropriate language. In general, as children grow they will be able to understand and process more information. Young children will mostly need to understand that problems are being addressed by their parents.
2. Give them reassurance that they did not cause it and are not responsible for fixing their parent’s problems.
3. It is also important to let them know that their parent’s problem is being treated effectively.
4. It’s especially important for kids to know that their parent has a problem but that it does not interfere with his or her love for them.
5. As much as possible provide unstressed time with the parent who is not suffering from symptoms of OCD. This can help them keeps things in perspective.
6. Keep their lives going along as normally as possible. School activities, sports and social events can help keep them connected even during difficult times.
7. As the parent with OCD improves, it is important for him or her to reinforce their relationship with the child. This will also provide stability, hope and optimism for facing the problems that will need to be faced in life.
8. Children are resilient. Everyone faces difficult times in life, including children, and we often gain confidence in our ability to handle the challenges of life when we get some practice as a child.
Managing Recovery & Preventing Relapse
While there has been significant progress in treating OCD, it is not a simple condition that can be completely cured. Instead, it is more like a chronic illness such as diabetes—manageable with the right care and treatment. Effective therapies, including Cognitive Behavioral Therapy (CBT), can help individuals lead fulfilling lives. However, long-term management is necessary, requiring awareness and dedication.
CBT has been shown to reduce OCD symptoms by up to 80%, helping individuals change their reactions to fear and uncertainty. However, since OCD is persistent, ongoing effort is required. Exposure and Response Prevention (ERP), a key part of CBT, involves confronting fears and resisting compulsive behaviors. This process may feel stressful, but it is essential for long-term improvement. OCD can also evolve over time, shifting from one type of obsession to another. Recognizing these changes can help individuals maintain control and prevent relapse.
Support from others can be valuable. Joining an OCD support group can reduce feelings of isolation and provide encouragement from those who have faced similar challenges. Being open about symptoms, although difficult, can help lessen shame and build confidence in managing OCD. Since recovery is not always a smooth path, having a relapse response plan can prevent discouragement. Setbacks are common, and feeling like a failure is unnecessary. A well-prepared plan can help individuals regain control without withdrawing from therapy.
OCD often leads to avoidance, meaning individuals may have lived with restrictions for a long time. Reclaiming responsibilities can feel overwhelming, and loved ones may also need time to adjust. Open conversations with family and friends can help manage these transitions. In some cases, therapy for couples or families may be beneficial in addressing concerns and strengthening support. Relapses may happen, but they do not erase progress. Each step forward builds resilience, making it easier to manage OCD in the long run.
Self-Care for Now and the Rest of Your Life
Taking care of your overall well-being is essential in managing OCD and preventing relapse. While it may feel like an extra burden, neglecting basic needs like nutrition, sleep, and exercise can make treatment feel overwhelming rather than freeing.
1. Prioritize the Basics: A balanced diet and proper hydration provide the energy needed for recovery. If unsure about nutrition, consult a specialist to develop healthy habits.
2. Sleep & Exercise: Lack of sleep worsens anxiety, and OCD symptoms can lead to isolation and inactivity. Regular exercise, even a simple walk, can improve mood and overall well-being. Address sleep issues with your doctor to ensure proper rest.
3. Make Time for Life: Spending time with loved ones and engaging in enjoyable activities helps reinforce the purpose of recovery. As OCD takes up less space in your life, you’ll have more time to truly live.
4. Follow-Up Care: Even when feeling better, staying in touch with your therapist helps maintain progress and prevent setbacks before they become major obstacles.
5. Plan for the Future: OCD may have consumed much of your time, but recovery allows you to focus on personal goals. Make meaningful plans for yourself and your loved ones to create a fulfilling future.
This concludes our 2 part series about OCD to help you and your loved ones understand it better and take informed decisions.
If you want to re-read or have missed the Part 1 to understand OCD, its Types, Related Disorders and Causes. READ HERE













