Understanding OCD: A Comprehensive Guide for Patients and Families
By Aarogya Minds
What is OCD ?
Rahul constantly worried about germs and contamination. He feared touching doorknobs, handling money, or being in public places, believing he could spread illness. He spent all day repeatedly washing his hands until they were raw and cleaning surfaces to ensure they were germ-free. After touching anything "dirty," he sanitized repeatedly and avoided eating food prepared by others. Rahul also avoided public restrooms and changed clothes multiple times a day. Despite his constant cleaning, he never felt completely clean or safe.
The key features of Obsessive-Compulsive Disorder are obsessions and compulsions. Most people have both, but for some it may seem as though they have only one or the other.
Obsessions: Intrusive, repetitive, distressing thoughts, images, or impulses.
Obsessions are thoughts, images, or urges. They can feel intrusive, repetitive, and distressing. Everyone has bothersome thoughts or worries sometimes (e.g. worry about money or whether or not we remembered to lock the front door, or regret over past mistakes). When a person is preoccupied with these thoughts, and is unable to control the thoughts, get rid of them, or ignore them, they may be obsessions. Obsessions are usually unrealistic and don’t make sense. Obsessions often don’t fit one’s personality; they can feel unacceptable or disgusting to the person who has them. Obsessions cause distress, usually in the form of anxiety. People with obsessive thoughts will often try to reduce this distress by acting out certain behaviours, known as rituals or compulsions.
Compulsions: Things a person does to ease the distress from obsessions.
Compulsions are behaviors a person does to relieve the distress they feel because of the obsessions. They can be overt (observable) or covert (hidden). While most people have preferred ways of doing certain things (e.g. a morning routine or a certain way to arrange items on a desk), people with OCD feel they “must“ perform their compulsions and find it almost impossible to stop. Usually, people with OCD know the compulsion is senseless. However, he or she feels helpless to stop doing it and may need to repeat the compulsion over and over again. Sometimes this is described as a ritual.
Common compulsions include excessive washing and checking, and mental rituals such as counting, repeating certain words, or praying. While compulsions often help relieve distress in the short-term, they don’t help in the long- term. As a person with OCD gets used to doing them, the rituals become less helpful at reducing his or her anxiety. To make them more effective again, the person may perform them more frequently and for longer periods of time. This is why people with OCD can appear to be “stuck” doing the same thing over and over again.
For someone with severe OCD, these compulsions can take up a considerable amount of time. Even simple tasks can become very time-consuming, having a significant impact on a person’s ability to manage their daily lives. These difficulties can result in significant shame, sadness, and frustration.
Obsessive-Compulsive disorder is common: about 2.5% of the population or 1 adult in 40 are afflicted, which makes it about twice as common as schizophrenia and bipolar disorder. It is also the fourth most common psychiatric disorder. It can be severe and debilitating: OCD can invade all aspects of a person’s life; family, work, and leisure can all be negatively impacted by the disorder. In fact, the World Health Organization (WHO) considers OCD to be one of the top 10 leading causes of disability out of all medical conditions worldwide.
Other facts about OCD:
It affects people from all cultures
Rates of OCD are equal in men and women
It can start at any age but typical age of onset is adolescence or early adulthood (childhood onset is not rare however)
Tends to be lifelong if left untreated
Common Obsessions
The list below provides examples of common obsessions but doesn’t cover the wide range of thoughts that OCD can include. Obsessions can be about anything... if you can think it, OCD can obsess about it.
Contamination
• Fear of contamination by germs, dirt, or other diseases (e.g. by touching an elevator button, shaking someone’s hand)
• Fear of saliva, feces, semen, or vaginal fluids.
2. Doubting
• Fear of not doing something right which could cause harm to one’s self or another (e.g. turning off the stove, locking the door)
• Fear of having done something that could result in harm (e.g. hitting someone with a car, bumping someone on the subway)
• Fear of making a mistake (e.g. in an email, or when paying a bill.
3. Ordering
• Fear of negative consequences if things are not “just right”, in the correct order or “exact” (e.g. shoes must be placed by the bed symmetrically and face north)
4. Religious
• Fear of having thoughts that go against one’s religion.
• Preoccupation with religious images and thoughts.
5. Aggressive
• Fear of harming others (e.g. harming a baby, stabbing someone with a kitchen knife, hurting someone’s feelings)
• Fear of harming self (e.g. jumping off a bridge, handling sharp objects)
• Fear of blurting out obscenities in public (e.g. saying something sacriligious in church)
6. Sexual
• Unwanted or forbidden sexual thoughts, images, or urges (e.g. urge to touch a parent in a sexually inappropriate way)
• Sexual thoughts involving children or incest.
Common Compulsions
Cleaning/Washing
• Washing hands too frequently or in a ritualized way
• Ritualized or excessive showering; bathing; grooming routines; cleaning of household items or other objects
• Although not a specific ritual, avoidance of objects or situations that are considered “contaminated” may be a major problem (e.g. will not shake hands with others or touch elevator buttons)
2. Checking
• Checking that nothing terrible did, or will, happen (e.g. checking driving routes to make sure you didn’t hit anyone with your car)
• Checking that you don’t make mistakes (e.g. rereading everything you have written, or asking others whether you said the “wrong” thing
3. Ordering/Arranging
• Ensuring that things are “just right” or consistent with a specific rule (e.g. everything in the kitchen must be perfectly lined up; can only wear certain coloured clothes on certain days)
4. Mental Rituals
• Needing to count to certain numbers, think certain ‘good’ or neutral thoughts in response to ‘bad’ thoughts, or pray repeatedly
5. Hoarding**
• Collecting “useless” items such as newspapers, magazines, bottles, or pieces of garbage
• Difficulty parting with unnecessary or excessive belongings (e.g. items that may have been useful once, or have sentimental value even though they are not needed, or are simply excessive, such as 30 black sweaters)
• Inability to throw these items away **Although hoarding used to be considered a feature of OCD, it is now thought of as a separate but related condition; See Below.
What are Obsessive-Compulsive Related Disorders?
There are several disorders that seem to be related to OCD. They share similar features such as intrusive thoughts and/or repetitive behaviours. Although similar, there are important differences to consider when looking at effective treatments.
Obsessive-Compulsive Related disorders include:
Body Dysmorphic Disorder
Trichotillomania (Hair-Pulling Disorder)
Excoriation (Skin- Picking) Disorder
Hoarding Disorder
These issues each seem to occur in about 1-4% of the general population, although there is speculation that hoarding may be far more common. Severity ranges but when they impair a person’s functioning or when they cause significant distress, treatment may be necessary.
1.Body Dysmorphic Disorder (BDD)
No matter how much her mother tried to convince her that it was not true, Alia really believed that she was ugly. At first she thought her skin was flawed, and then that her nose was too large. Later, whenever she looked in the mirror, she was convinced that she was so disturbing for others to look at that she avoided going out in public.
People with BDD are overly concerned about an imagined or minor flaw in their appearance. The focus of concern is often the face and head, but other body parts can become a focus. While most people would probably like to change one or two aspects of their appearance, people with BDD are very preoccupied with these issues. They feel intense distress as a result. For many, the concern can cause serious impairment in their day-to-day lives. BDD is considered by mental health professionals to be in the same category of conditions as as OCD, due to their similarity. For example, BDD involves intrusive and recurrent thoughts about one’s appearance as well as compulsive behaviours to ease the distress of these thoughts. A person may be very concerned by the shape or size of their nose and repetitively check mirrors, ask for reassurance, or consult with cosmetic surgeons in attempts to relieve their distress. Like the compulsions in OCD, these behaviours may provide short-term relief (e.g. “my nose doesn’t look too bad in that mirror”) but make things worse in the long run (e.g. increase need to check mirrors).
Body Dysmorphic Disorder (BDD): preoccupation with an imagined or slight flaw in one’s appearance. BDD often includes repetitive behaviors that are done in response to appearance concerns.
2. Trichotillomania (also known as Hair-Pulling Disorder)
Trichotillomania involves recurrent hair pulling, resulting in noticeable hair loss. People with compulsive hair pulling may pull hair from any part of their body, including the scalp, eyebrows, eyelashes, pubic area, and legs. Severity ranges broadly: for some, thinning areas are visible only upon close inspection, while others pull to the point of baldness. For some, the urge to pull can be managed with simple tools like relaxation and increased awareness. For others, the urge can be so strong at times that it feels impossible to resist. Many people wear wigs, hats, or scarves to disguise the hair loss on their scalp, while others may use make-up or false eyelashes for hair loss in other areas. The repetitive nature of pulling seems similar to compulsions in OCD. However, the pulling is usually done for different reasons. For some, the need to pull happens in response to feelings of tension which are relieved after pulling. For others, pulling seems to happen automatically with little awareness and no sense of tension or relief.
Trichotillomania (Hair-pulling Disorder): compulsive hair pulling to the point of noticeable hair loss.
3. Excoriation (Skin- Picking) Disorder
Similar to hair pulling, skin picking is thought to be compulsive when it becomes recurrent and results in noticeable scarring and/or damage to the skin. People with compulsive skin picking will make repeated efforts to stop or reduce their picking, and are significantly distressed by their behaviour. Skin picking can occur on any part of the body, including the face, scalp, lips, and legs. While it is often done in response to a perceived imperfection, this is not always the case. Regardless, compulsive picking results in pain and damage to the skin.
Excoriation (Skin-Picking) Disorder: compulsive skin-picking resulting in noticeable damage to the skin.
4. Hoarding Disorder

Photo depecting Hoarding Disorder
People with hoarding disorder have trouble with stuff. They acquire too much stuff and/or have trouble getting rid of it. The types of things that people hoard can vary but are often perceived as potentially useful in the future, valuable or as having sentimental value. Like all the disorders described here, saving and collecting occurs on a continuum. Most people save some items that they consider useful or sentimental but when a space becomes cluttered enough to compromise intended use (e.g. unable to sit on couch in living room due to clutter) or the person is unable to maintain a safe environment for themselves and others, a diagnosis and treatment may be warranted. Potential risks of hoarding include fires, falls, blocked entrances and exits, infestation with rodents and insects, lung disease, and inability to maintain good hygiene. Hoarding shares some similar features with OCD: some people describe obsessional thinking about their belongings and a compulsive need to acquire items. Also, the distress felt when having to resist acquiring or when discarding items is considered similar to the anxiety in OCD. However, the thoughts are not typically described as intrusive or distressing and the behaviour is not ritualistic and is often considered pleasurable.
Hoarding Disorder (HD): Persistent difficulty getting rid of possessions because of a perceived need to save them.
How Do We Know it’s OCD? Assessment & Diagnosis
Everyone will have upsetting thoughts and many people have certain ways of doing things. For most, these thoughts and behaviours are not a problem. What makes someone with OCD different? Assessment and diagnosis of OCD involves making the distinction between normal thoughts and behaviours and a diagnosable condition. The big distinctions are the amount of time occupied by obsessions and compulsions, the degree of distress, and/or the level of impairment (e.g. difficulty attending work or school, or inability to socialize).
The American Psychiatric Association (APA) defines OCD in the following way:
The presence of obsessions and/or compulsions which occupy more than one hour per day, cause marked distress OR significantly interfere with functioning.
• Obsessions
·· Persistent unwanted thoughts, images, or impulses
·· Intrusive, uncontrollable/excessive ·· provoke anxiety
• Compulsions
·· Repetitive behaviours or mental acts
·· Performed in response to an obsession, or in ritualistic fashion
·· Intended to reduce discomfort or prevent feared event.
Mental health professionals use specific interview strategies and questionnaires to determine whether or not a person has OCD. Clinicians are careful to ensure that a person’s symptoms are not better accounted for by a different problem, clinicians are careful to “rule out” other possibilities. For example, many anxiety disorders have similarities: fear of specific situations or things; avoidance; severe anxiety.
Sometimes individuals dealing with depression will become intensely preoccupied with thoughts regarding their past failures. Accurate assessment is important because it helps guides treatment. Different challenges require different solutions. It is also important to note that OCD can also occur at the same time as other disorders. Sometimes a clinician may determine that one problem is “primary” which may mean it needs to be treated first before other disorders can be addressed.
As mentioned, OCD is similar to other disorders in some ways. Below is a list of disorders that are commonly confused with, or can occur at the same time as OCD. It may be useful to talk to your healthcare provider about the differences in more detail to make sure you find the right help.
Common Anxiety Disorders
• Panic disorder (fear of recurrent, unexpected panic attacks)
• Agoraphobia (fear of specific situations such as buses or trains, crowded places or of leaving home alone)
• Generalized Anxiety Disorder (excessive worry about real-life concerns, e.g. health or money)
• Social Phobia (fear of scrutiny, humiliation or embarrassment in social situations)
• Specific Phobia (fear of a particular object or situation, such as heights or snakes)
• Post-traumatic Stress Disorder (the re-experience of fear following a traumatic event)
• Anxiety disorder due to a general medical condition (anxiety symptoms are directly related to a medical condition; can be ruled out by physician’s exam)
• Substance-induced anxiety disorder (anxiety directly related to the effects of a substance, such as cocaine)
How Do People Get OCD? Causes of OCD
Like most psychiatric conditions, research indicates that there is no single cause of OCD. Instead, most experts agree that OCD is likely caused by a combination of biological, psychological, and sociocultural factors.
1.Changes in Brain Chemistry
Chemical messengers in the brain, known as neurotransmitters, transmit signals between brain cells (neurons). These signals are the biological basis in the brain for most of our experiences, like mood, sleep, memory and learning. Some of these neurotransmitters are believed to play a large role in the development of OCD, hoarding, trichotillomania, compulsive skin picking, and other related disorders. Serotonin, for example, is a neurotransmitter that is important in the regulation of mood and impulse control. It also affects memory and learning processes. There seems to be a link between decreased levels of available serotonin in certain brain areas and the development of OCD, as well as other conditions such as depression and anxiety disorders. The antidepressant medications used to treat OCD work by raising the level of this messenger in the brain. Dopamine is an important neurotransmitter for the reward systems in the brain, and has also been linked to OCD, and similarly antipsychotic medications which affect dopamine can also sometimes be helpful to OCD. Another major neurotransmitter, glutamate, is now being investigated in its role in the development of OCD.
2. Changes in Brain Activity
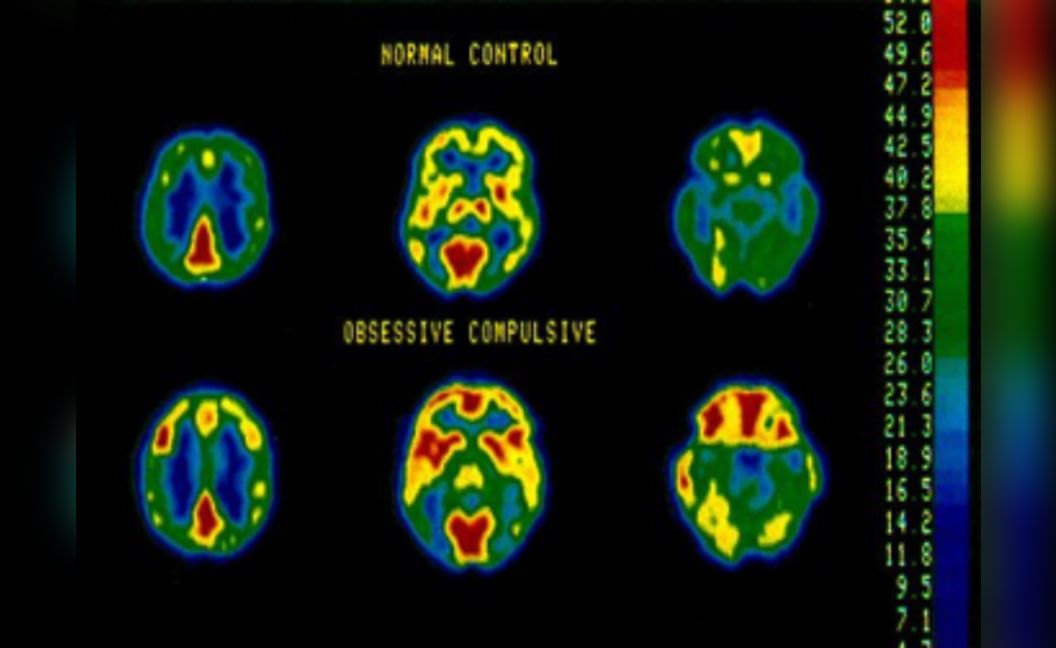
Brain scans show increased activity in OCD (bottom) compared to a normal brain (top), highlighting hyperactivity in key regions.
Researchers and clinicians are able to study the levels of brain activity, or metabolism, with advanced imaging techniques such as Positron Emission Tomography (PET), Single Photon Emission Computed Tomography (SPECT) and functional Magnetic Resonance Imaging (fMRI). Such studies have consistently shown that individuals with OCD have increased levels of activity in three areas of the brain: the basal ganglia, prefrontal cortex, and cingulate gyrus.
The caudate nucleus is a deep brain structure located in the basal ganglia. It is believed to act as a filter, screening messages that it receives from other areas of the brain. It also regulates habitual and repetitive behaviors, such as those observed in OCD and related disorders. Interestingly, the increased level of brain activity in this area normalizes in individuals after successful treatment of OCD, either with medications or cognitive behavior therapy. This demonstrates that changes in ‘thinking’ that occur in therapy can alter physical functions in the brain.
The prefrontal cortex is another structure implicated in OCD. It is involved in regulating appropriate social behavior. Diminished activity in this area can lead to poor impulse control, impaired judgment and lack of remorse. Increased activity may therefore be related to increased worry about social and moral concerns, such as meticulousness, cleanliness and fears of being inappropriate, all of which are amplified in OCD.
The cingulate gyrus helps regulate emotion. It is also involved in predicting and avoiding negative outcomes, and recognizing errors. In OCD, increased activity in this brain region may be related to the emotions triggered by obsessive thoughts and to feelings that one has made a mistake or not done something correctly. This area is well connected to the prefrontal cortex and basal ganglia via a number of brain circuits.
3. Genetic Factors in OCD
It is widely agreed that OCD and its related disorders can run in families. Almost half of all cases demonstrate this pattern. Studies show a higher likelihood that close relatives of a person with OCD (e.g. parents, siblings or children) have or will develop the disorder at some point in their lifetimes. Although OCD symptoms can be ‘learned’ from affected family members, relatives with OCD often have different obsessions and compulsions.
There is also a relationship between OCD and Tourette’s syndrome (TS). Family members of individuals with TS often show higher rates of OCD than the general population, also suggesting a genetic relationship between these disorders.
There is a lot of interest in the exact genes involved in OCD. Such potential gene ‘candidates’ may include genes that are involved in the regulation of serotonin and other brain chemicals. At this point in time, although changes in specific genes have been identified that may contribute to the risk of the illness, the effect of of these variants is too small to be clinically helpful. However in the near future gene testing may be able to help better predict the future course of the illness, or response to treatment.
4. Psychological Factors
A. Cognitive Theory
Cognitive (i.e. thought processes) theory focuses mainly on the thoughts in OCD, instead of the behaviours. It is based on the idea that thoughts impact how we feel. In OCD, this theory suggests that people with OCD misinterpret their thoughts. It is not the obsession itself that is the problem, it is the way the obsession is interpreted.
Cognitive theorists have identified several patterns of beliefs that are common in OCD. They may contribute to the ways people with OCD misinterpret their thoughts.
• Over-inflated sense of responsibility : the belief that you are solely responsible for preventing harm to others.
• Exaggerated sense of threat: a tendency to overestimate the likelihood of danger
• Over-importance of thoughts: thoughts are very important and must be controlled
• Thought-action fusion: just having a thought increases the chances that it will come true and/ or that I will act on it • Perfectionism: mistakes are unacceptable
• Intolerance of Uncertainty: a need for 100% certainty about a given situation
B. Behavioural Theory
Unlike cognitive therapy, which looks at thoughts, behaviour theory focuses on the behaviours in OCD. According to behaviour theory OCD makes connections between certain situations and fear (e.g. public bathroom = anxiety). In order to reduce that fear, the person learns to avoid those situations or do rituals. A link is formed between the compulsion and feeling better. The more someone avoids or ritualizes in response to this fear, the stronger that link becomes. The stronger this connection, the more likely a person is to continue their avoidance or rituals because they don’t have to confront or tolerate that distress... Their avoidance or compulsions become reinforced and the association may start to get triggered in other similar situations like bank machines or public handrails.
C. Social and Cultural Factors
Research on OCD in different cultural groups suggests that there are no big differences across cultures, age, or between genders. Instead, OCD symptoms often seem related to the things we value most or that are particularly relevant in our lives. For example, obsessions about harming one’s baby is common amongst new parents with OCD. Similarly, individuals raised in religious homes may develop obsessions that seem to contradict one’s religious beliefs (e.g. sexual thoughts about God).
This concludes Part 1 of our guide to understand OCD. In next and final part we discuss Treatment Options for OCD, How Do We Manage Recovery and Prevent Relapse? and How does effect Family and Friends?. You can read the Part 2 here.













